Interventional pain management represents a shift in the approach to chronic pain, a condition affecting at least 100 million Americans. This specialized field uses minimally invasive procedures not just to alleviate pain, but to fundamentally improve the quality of life for patients suffering from persistent ache conditions.
IPM is relatively recent, with its roots tracing back to 1899, marked by the advent of regional analgesia and nerve blocks. However, it wasn’t until 1996 that the term “interventional pain management” was coined by Steven D. Waldman, signifying a new era in treating pain.
That is why we believe is important to talk about important things like:
- IPM aims not only to alleviate aches but also to enhance the quality of life for patients suffering from persistent conditions.
- The procedures in IPM are minimally invasive, aiming to provide significant relief with minimal risk and recovery time.
- IPM specialists are trained in a variety of techniques and procedures. They focus on personalized treatment plans and are responsible for educating patients about their conditions and treatment options.
Now, let us take a look at the most important factors regarding this concept.
Procedures and Treatments
Interventional pain management employs a variety of procedures to treat pain effectively.
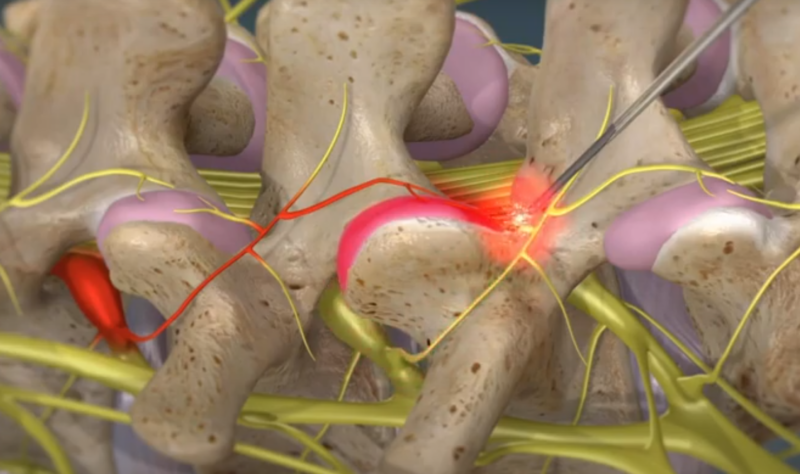
Radiofrequency Nerve Ablation
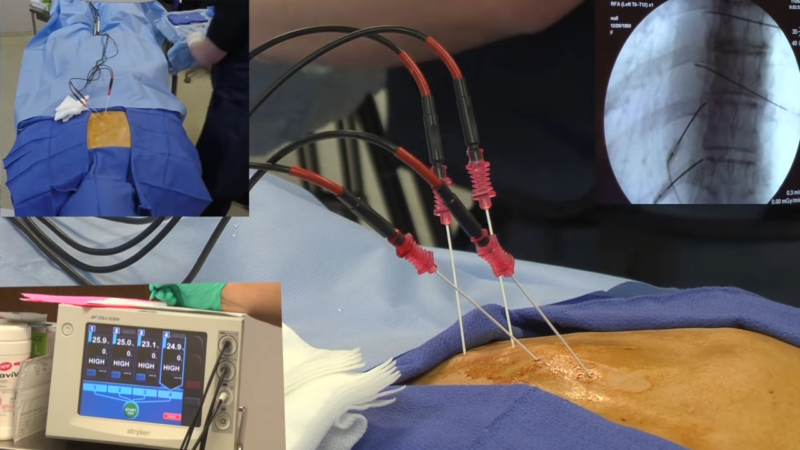
- Technique: Uses radiofrequency waves to heat and destroy nerve tissue.
- Purpose: Reduces ache signals from the targeted area.
- Applications: Effective for chronic aches, especially from arthritis.
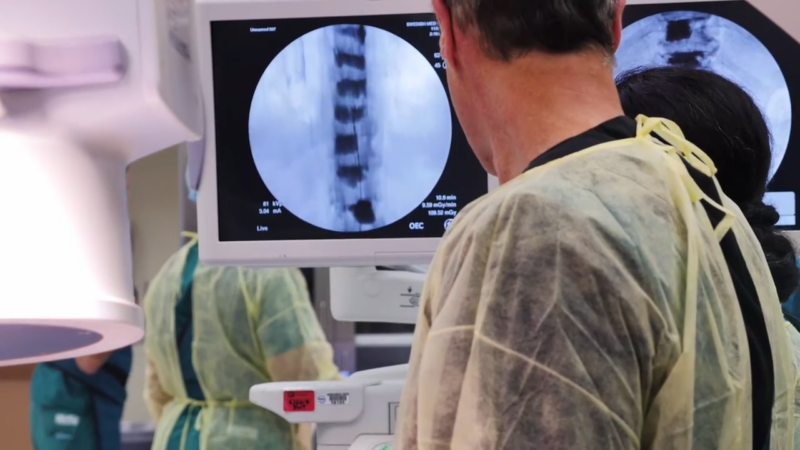
- Guidance Method: X-ray imaging for precision.
Discography
- Technique: Injection of contrast dye into spinal discs.
- Purpose: Diagnoses the cause of back ache by identifying sources in the discs.
- Applications: Crucial for guiding treatment of back ache.
Percutaneous Discectomy/Nucleoplasty
- Technique: Removal of tissue from spinal disc.
- Purpose: Relieves pressure in the spine.
- Applications: Treatment for certain types of back ache.
Steroid Injections

- Technique: Injection of steroids into specific aceh points.
- Purpose: Reduces inflammation and alleviates pain.
- Applications: Commonly used for muscle, joint ache, and osteoarthritis.
Pain Pump
- Technique: Surgically implanted device delivering pain medication.
- Purpose: Offers targeted ache relief directly at the ache site.
- Applications: Beneficial for patients needing constant pain management.
Nerve, Root, and Medial Branch Blocks
- Technique: Injection that interrupts nerve-to-brain pain signals.
- Purpose: Provides relief from chronic pain; diagnostic tool.
- Applications: Identifying and treating specific ache sources.
Rhizotomy
- Technique: Use of heated electrodes to disable specific nerves.
- Purpose: Effectively “turns off” pain signals.
- Applications: Treatment for chronic pain conditions.
Spinal Cord Stimulation
- Technique: Uses electrical currents to block ache perception.
- Purpose: Alters pain signals sent to the brain.
- Applications: Varied, for different types of chronic pain conditions.
Interventional Pain Management Techniques
Interventional pain management encompasses a range of techniques designed to target the specific mechanisms of ache. These techniques are minimally invasive, aiming to provide significant pain relief with minimal risk and recovery time.
Nerve Blocks
Nerve blocks are a primary method in IPM. They involve injecting anesthetic or anti-inflammatory medication near specific nerves. This can provide temporary or prolonged relief from ache by interrupting the transmission of pain signals to the brain.
Radiofrequency Ablation
Radiofrequency ablation uses heat generated from radio waves to disable specific nerve fibers responsible for transmitting ache signals. This technique is particularly effective for chronic conditions like arthritis, providing relief in areas such as the lower back and neck.
Spinal Cord Stimulation
Spinal cord stimulation employs electrical currents to interfere with pain signal transmission. This method is beneficial for chronic ache conditions, offering relief by altering the way pain signals are sent to the brain.
Injections
Interventional pain management often includes various types of injections. These include epidural steroid injections, facet joint injections, and trigger point injections, delivering medication directly to the pain source to reduce inflammation and provide relief.
Pain Pumps and Implantable Drug Delivery Systems
Pain pumps and implantable drug delivery systems allow for the direct delivery of pain medication to the ache site. This minimizes the need for oral medications and reduces potential side effects.
Peripheral Nerve Field Stimulation
Peripheral nerve field stimulation, related to spinal cord stimulation, is used for ache localized in other body parts. It involves placing electrical leads near the ache source to disrupt pain signals, providing targeted ache relief.
Role of Interventional Pain Management Specialists
The role of Interventional Pain Management (IPM) specialists is multifaceted and essential in the field of pain medicine. These professionals are not just clinicians but also educators, advisors, and innovators in managing chronic and acute pain. Here’s a view of their role:
- Expert Diagnosis and Treatment: IPM specialists possess deep knowledge in diagnosing various pain conditions. They use advanced diagnostic tools and techniques to accurately pinpoint the sources of pain.
- Personalized Care Plans: Recognizing that pain is a subjective and complex experience, IPM specialists prioritize creating personalized care plans. They consider factors like the patient’s pain history, lifestyle, response to previous treatments, and overall health.
- Multi-Disciplinary Collaboration: A significant aspect of their role involves working in a multidisciplinary team. This team may include other medical specialists, physical therapists, psychologists, and nurses.
- Patient Education and Communication: Education is a critical component of their role. IPM specialists spend considerable time discussing with patients about their conditions, explaining the nature of the pain, and outlining various treatment options.
The Science Behind Pain
Understanding the science behind pain is essential in appreciating the effectiveness of IPM. The neuroscience of ache reveals that it involves an intricate network within the brain and nerves. When ache is experienced, nerve cells in the affected tissue send signals to the brain, activating a large network, including the dorsal anterior cingulate cortex (dACC).
The dACC plays a critical role in the processing and modulation of ache. It acts like a control center, regulating the intensity and emotional response to pain. This understanding is crucial for interventional ache management, as it allows for targeted treatments that can modulate these pain signals.
By intervening at specific points in the ache transmission pathway, these treatments can effectively reduce the perception of pain, thereby alleviating suffering and improving the patient’s quality of life. An insight into the neuroscience of ache forms the foundation upon which IPM builds its varied and effective treatment strategies.
FAQs
What is non-interventional pain management?
Non-interventional pain management involves techniques that do not require invasive procedures, such as medications, physical therapy, and psychological support.
What are complications of interventional pain procedures?
Complications can include infection, bleeding, nerve damage, and allergic reactions to medications or materials used.
What are the three levels of pain management?
General measures like over-the-counter medication and lifestyle changes, specialist interventions like physical therapy, prescription drugs, and advanced care involving multidisciplinary teams and possibly surgery.
What is a non-interventional?
A non-interventional approach refers to treatments or studies that do not involve active manipulation or intervention, such as observational research or non-invasive therapies.
Summary
IPM approach is often used when pain is severe or chronic and has not responded to more conservative treatments like medication or physical therapy.
The goal of IPM is to relieve, reduce, or manage pain and improve a patient’s overall quality of life through minimally invasive therapies that are specifically designed to diagnose and treat painful conditions.
This specialty also emphasizes the importance of a comprehensive approach, often involving a multidisciplinary team, to address the physical, emotional, and psychological aspects of pain.